HEARING LOSS
Three Major Causes of
Hearing Loss
Genetic Hearing Loss
 Genetics is one of the most common causes of hearing loss accounting for 30% to 50% of all hearing loss and approximately 60 percent of deafness occurring in infants.
Genetics is one of the most common causes of hearing loss accounting for 30% to 50% of all hearing loss and approximately 60 percent of deafness occurring in infants.
Age Related Hearing Loss
Age-related hearing loss (presbycusis) gradually occurs in most of us as we grow older. It is one of the most common conditions affecting older and elderly adults.
Noise-Induced Hearing Loss
 Every day, we experience sounds in our environment, such as the sounds from television and radio, household appliances, and traffic.
Every day, we experience sounds in our environment, such as the sounds from television and radio, household appliances, and traffic.
hearing loss
Five Important Definitions of Hearing Loss
As no two individuals experience hearing loss in exactly the same way,
there are a multitude of factors that can contribute to this condition.
Congenital Hearing Loss
Present at birth e.g. congenital hearing loss or deafness.
Sensorineural Hearing Loss
A type of hearing loss that occurs when there is damage to the inner ear or the neural pathways that transmit sound to the brain.
Conductive Hearing Loss
Caused when sound is not conducted properly through the outer ear to the eardrum.
Syndromic Hearing Loss
Refers to hearing loss that is associated with other medical conditions or syndromes, which may affect various parts of the body in addition to the ears.
Non-Syndromic Hearing Loss
Refers to a hearing impairment that accounts for the majority of genetic-related hearing loss, nearly 70 percent.
hearing loss
How Do We Hear?

Sound waves enter the outer ear and travel through a narrow passageway called the ear canal, which leads to the eardrum.

The eardrum vibrates from the incoming sound waves and sends these vibrations to three tiny bones in the middle ear. These bones are called the malleus, incus, and stapes.

The bones in the middle ear couple the sound vibrations from the air with fluid vibrations in the cochlea of the inner ear, which is shaped like a snail and filled with fluid. An elastic partition runs from the beginning to the end of the cochlea, splitting it into upper and lower parts. This partition is called the basilar membrane because it serves as the base, or ground floor, on which key hearing structures sit.

Once the vibrations cause the fluid inside the cochlea to ripple, traveling waves form along the basilar membrane. Hair cells, (sensory cells sitting on top of the basilar membrane), ride the wave.

As the hair cells move up and down, microscopic hair-like projections (known as stereocilia) that perch on top of the hair cells, bump against an overlying structure and bend. Bending causes pore-like channels, which are at the tips of the stereocilia, to open up. When that happens, chemicals rush into the cells, creating an electrical signal.
Ringing in your ears?
What is Tinnitus?
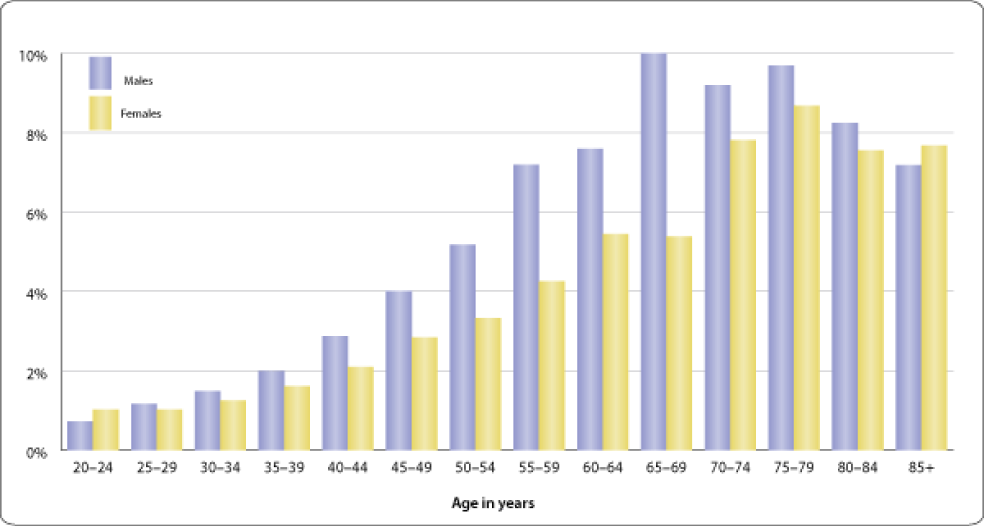
This chart shows age and sex-specific trends in chronic tinnitus, i.e., ringing, roaring, or buzzing in the ears or head that has lasted for 3 months or longer in the past year. This information was collected in household interviews conducted as part of the 1994–1995 Disability Supplement to the U.S. National Health Interview Survey; the data are self-reported and exclude proxy responses.
The overall trend with age shows a marked increase for both sexes, beginning at age 40, peaking between 65 to 79 years, and then declining after 80 years of age. Males show significantly higher rates of tinnitus (p<0.0001) compared to females. The male prevalence is consistently higher from age 40 through 79 years, with the largest differences between males and females occurring from 50 through 69 years of age.
One explanation for these differences is that males are more likely to be exposed to loud environmental noise, whether through work or leisure activities. Strong associations between occupational noise exposure and tinnitus are well documented in the literature (Hoffman and Reed, 2004).
Who is affected by NIHL?
Noise-induced hearing loss can affect anyone who is exposed to loud noises, but individuals who work in noisy environments such as construction sites, factories, and music venues are at a higher risk of developing the condition.
Why do we lose our hearing as we get older?
As we age, the tiny hair cells within our inner ear that are responsible for detecting sound begin to deteriorate and die off. This leads to a gradual loss of hearing ability, known as presbycusis, which typically affects high-frequency sounds first.
